Dementia is a general term used to describe a number of brain diseases that lead to a decline in mental and psychological function. All types of dementia can be debilitating and destructive. Nursing diagnosis is important in caring for patients with dementia.
It is most commonly associated with Alzheimer’s disease, but can also be caused by vascular dementia, Lewy body dementia, Alcohol-related dementia, and frontotemporal dementia.
In this article, we will be discussing nursing diagnosis for dementia. This is a complex and important topic, as dementia affects millions of people all over the world.
We will start by discussing the basics of neuropathology- what happens in the brain when someone develops Alzheimer’s disease or vascular dementia.
Then we will move on to discuss the different stages of dementia, and how to make a diagnosis.
Finally, we will look at some of the most common responsive behaviours seen in people with dementia, and ways to support them and their carers.
The Increasing Prevalence Of Dementia
Someone in the world develops dementia every 3 seconds. There are over 55 million people worldwide living with dementia in 2020. This number will almost double every 20 years, reaching 78 million in 2030 and 139 million in 2050.
Much of the increase will be in developing countries. Already 60% of people with dementia live in low and middle-income countries, but by 2050 this will rise to 71%. The fastest growth in the elderly population is taking place in China, India, and their south Asian and western Pacific neighbours.
In 2019 an estimated 447,115 Australians were living with dementia. Without a medical breakthrough, this figure is expected to increase to almost 1.1 million by 2058.
In Australian hospitals, approximately 20-25% of patients over the age of 70 years have dementia and this figure increases to 47% in patients aged 90 years and over. The actual incidence is likely to be higher because cognitive impairment (dementia and delirium) is under-recognised in hospitals and dementia is under-diagnosed in the community.
What Is Dementia?
Dementia is not one specific disease; it’s often described as an umbrella term. The term ‘dementia’ describes a neurodegenerative syndrome that may be caused by any one of over 100 different diseases in which structural and chemical changes occur in the brain leading to brain tissue death. Dementia has no cure.
As a syndrome, dementia involves a progressive decline in language, memory, perception, personality and behaviour. It affects the person’s ability to perform everyday tasks and interferes with the person’s normal social and working life. The type of dementia someone has is generally named in accordance with the suspected underlying disease pathology. A dementia diagnosis is primarily established through a process of exclusion in which all other reversible physical and psychological causes are eliminated.
What Causes Dementia?
Alzheimer’s disease is the most common type of dementia in which amyloid plaques and neurofibrillary tangles in the brain disrupt communication between neurons causing their degeneration and death. It is a progressive disease that starts with short-term memory loss and gradually gets worse over time.
Vascular dementia is the second most common form of dementia and is caused by cerebrovascular conditions such as stroke and TIA. This can happen as a result of a stroke, or mini-strokes (known as transient ischaemic attacks).
Lewy body dementia is caused by the buildup of abnormal proteins in the brain, known as Lewy bodies. These proteins damage nerve cells and lead to problems with thinking, movement, behaviour and sleep.
Alcohol-related dementia also referred to as alcohol-related brain injury or alcohol-related brain impairment, results from excessive consumption of alcohol over many years. It affects memory, learning, reasoning and other mental functions, as well as personality, mood and social skills.
Frontotemporal dementia is caused by damage to the frontal and temporal lobes of the brain. This can lead to changes in behaviour, personality and language skills.
Parkinson’s disease causes problems with movement, but can also lead to dementia in around 20% of cases. This is known as Parkinson’s disease dementia.
There are many other causes of dementia, including Huntington’s disease, Creutzfeldt-Jakob disease and normal pressure hydrocephalus. However, these are much less common than the four main types we have discussed.
What Are The Symptoms Of Dementia?
The symptoms of dementia vary depending on the type of dementia, and the area of the brain that is affected.
However, there are some common symptoms that are seen in most types of dementia. These include:
- Cognitive impairment
- Impaired verbal communication
- Problems with thinking and reasoning
- Difficulty with planning and organisation
- Changes in mood and behaviour
Symptoms of Alzheimer’s Disease And Dementia
People with early-stage Alzheimer’s disease may have difficulty remembering recent events, but they can still hold a conversation and remember events from the past.
As the disease progresses, they may become withdrawn and lose interest in hobbies and activities. They may also have trouble recognising loved ones and struggle to find the right words when speaking.
In the late stages of Alzheimer’s disease, people may need help with all aspects of daily life, including eating, dressing and going to the toilet.
Symptoms Of Vascular Dementia
People with vascular dementia often have sudden onset symptoms after a stroke or TIA.
Symptoms vary depending on the location and extent of damage and may be sudden or gradual in onset. Symptoms in the early stages are similar to Alzheimer’s disease, but memory loss is not as great and mood fluctuations are more prominent.
Symptoms Of Lewy Body Dementia
People with Lewy body dementia may have hallucinations and problems with movement. They may also experience sudden changes in mood and levels of alertness.
Like Alzheimer’s disease, the symptoms of Lewy body dementia tend to get worse over time.
Symptoms Of Alcohol-Related Dementia
People with alcohol-related dementia have problems with memory, thinking and reasoning. They may also have problems with movement, balance and coordination.
Personality changes are common, and people may become withdrawn, depressed or anxious.
Symptoms Of Frontotemporal Dementia
People with frontotemporal dementia often have changes in their personalities and behaviours. They may become more impulsive, irritable or aggressive.
They may also lose interest in hobbies and activities, and withdraw from social situations.
Symptoms Of Parkinson’s Disease Dementia
The symptoms of Parkinson’s disease dementia are similar to those of Lewy body dementia, but they also include problems with movement.
People with Parkinson’s disease often have a tremor or shaking, in their hands and arms. They may also have problems with balance and coordination.
As the disease progresses, they may have difficulty speaking and swallowing.
In the late stages of Parkinson’s disease dementia, people may be unable to walk or care for themselves.
The Basic Neuropathology Of Alzheimer’s Disease And Vascular Dementia
Alzheimer’s Disease
When neural tissue is examined at the microscopic level there are three neuropathological hallmarks of Alzheimer’s disease which contribute to cell dysfunction and death:
1) Plaques that sit outside the neurons (Beta-Amyloid Proteins or Amyloid Plaques) are clumps of insoluble peptides caused by abnormal cleaving (splitting in the wrong spot) of the amyloid precursor protein.
2) Neurofibrillary tangles occur inside the neurons and are caused by the modification of a supporting protein called tau protein.
3) Neuronal degeneration. These are changes that can be seen to some degree in normal ageing, however, in people with Alzheimer’s Disease, the degree to which they occur is far more significant.
Vascular dementia
The second most common form of dementia is Vascular dementia, which represents several conditions characterised by compromise to the cerebral circulation. Ischaemic infarcts are the most common cause, although dementia can also result from haemorrhagic causes. The pattern of symptoms relates to the area and extent of the damage.
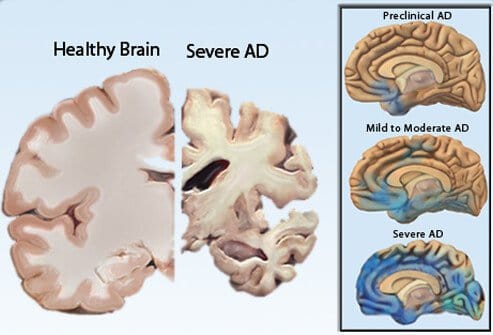
What Does The Brain Dementia Neuronal Destruction Look Like?
The development and infiltration of plaques and tangles commonly seen in dementia result in neuronal death. As neurons die the brain gradually reduces in size in the affected areas.
The Regions Of The Brain
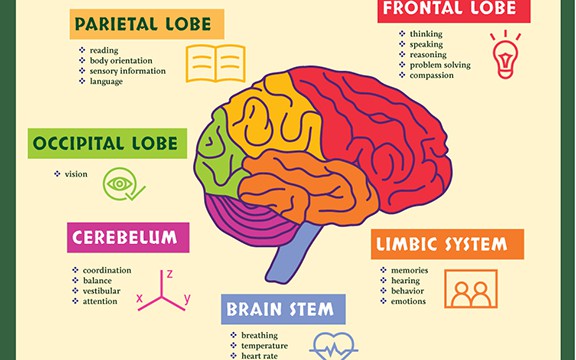
Here are examples of how damage to particular regions of the brain may give rise to cognitive difficulties and explain the patient’s responses and behaviours in the clinical environment.
Frontal Lobe
Responsible for planning, organisation and delegation, initiative, coordination, social and behavioural control, and impulse control (responding appropriately).
Parietal Lobe
Responsible for calculation, spatial reasoning, recognition and components of language (including reading, writing, speaking plus tone, melody, and intonation).
Occipital Lobe
Responsible for visual processing and discrimination of movement and colour.
Temporal Lobe
Responsible for memory (filing and retrieval), and language components including comprehension (Wernicke’s area) and motor aspects of speech (Broca’s area).
Limbic Region
Responsible for consciousness, sleep, appetite, emotions and forming memories.
Diagnostic Examination Of Alzheimer’s Disease And Dementia
The clinical history is the most important part of the diagnostic examination. The physician will ask about the patient’s medical history, family history, and symptoms.
Cognitive function testing can help understand the patient’s mental status and assess the patient’s functional ability, and a physical examination will be done. This may include a neurological exam and tests of blood, urine, and other body fluids.
Imaging tests may be done to look for plaques and tangles in the brain. These tests may include computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET).
A lumbar puncture (spinal tap) may be done to look for abnormal proteins in the cerebrospinal fluid.
Genetic testing may be done to look for changes in the genes that are linked to Alzheimer’s disease. The doctor may also do tests to rule out other conditions that can cause dementia.
Stages Of Dementia
There are seven stages of dementia, ranging from no impairment to severe impairment.
The first stage is no cognitive or functional impairments. In this stage, a person has no symptoms and functions normally.
The second stage is very mild cognitive impairment. A person in this stage may have some trouble remembering the names of their family members or recent events, but will still function relatively normally.
The third stage is mild cognitive decline. A person in this stage may have difficulty remembering names and faces, as well as recent events. They may also have trouble with planning and decision-making.
The fourth stage is moderate cognitive impairment. A person in this stage may have trouble with short-term memory, as well as difficulty understanding and using verbal language.
The fifth stage is severe cognitive impairment. A person in this stage may have trouble with short-term memory, as well as difficulty understanding and using verbal language. They may also have difficulty with movement.
The sixth stage is very severe cognitive decline. A person in this stage may be unable to communicate, as well as have difficulty with movement.
The seventh and final stage is complete cognitive and functional impairments. A person in this stage is unable to communicate or interact with their environment in any way. This is the most severe stage of dementia.
Responsive Behaviours Of Dementia
As discussed above, the neuropathology of dementia involves significant damage to the brain, affecting brain function.
As a result, each person with dementia experiences neurological deficits and these may vary widely between patients depending on which region of the brain is affected.
In most cases, as dementia progresses, responsive behaviours may also develop.
What Are Responsive Behaviours
Responsive behaviours are defined as symptoms of disturbed perception, thought content, mood, and behaviour that are present in people with dementia.
These often distressing symptoms include:
- Confusion
- Agitation
- Aggression
- Repetitive vocalisations
- Wandering
- Apathy
- Depression
- Hallucination and delusions
- Sexually and socially inappropriate behaviours
- Evening restlessness
While responsive behaviours are attributable to changes in the structure and chemistry of the brain, they may also be understood in terms of the attempts that the person with dementia makes to deal with unresolved psychosocial, physical and environmental stressors.
How Can We Help?
Responsive behaviours are not inevitable and may be prevented or reduced using therapies that focus on responding to each person’s individual situation.
Effective responses depend upon a detailed assessment of the individual, the behaviour and the context in which the symptoms are occurring. These symptoms can present as unmet needs or problems for the person and require support that focuses on reducing the behaviour within the context of the person’s individual situation.
Management strategies can include psychosocial, environmental and pharmacological strategies and often include a combination of these. Except in cases where the person is in extreme distress or at risk of harm to themselves or others, it is recommended that psychosocial measures and environmental triggers are attended to first.
The use of the term BPSD was recommended by a consensus group of the International Psychogeriatric Association (IPA) in 2002.
Prior to this, symptoms of dementia were not described consistently and negative connotations about the person with dementia were sometimes inferred from commonly used terms such as ‘problem behaviours’ or ‘behavioural disturbances’.
It is always important to remember to value and attempt to understand the person behind the behaviour and not see the behaviour as the person.
Adopting the ‘view from here may be helpful in coming to an understanding of the person’s perspective. It is also important to understand that responsive behaviours often contribute to significant carer and family stress and are the main reason people with dementia are placed into residential care.
Prevention of and/or an early response to responsive behaviours offers the best chance to alleviate suffering and improve the quality of life for the person with dementia as well as for their family and carers.
Nursing Diagnosis Of Dementia
Regardless of the cause, all types of dementia can be debilitating and destructive. Nursing diagnosis is important in caring for patients with dementia.
Dementia is a serious condition that can have a profound impact on patients and their families. With proper diagnosis and treatment, however, many people with dementia can enjoy a good quality of life.
Here are 3 examples of changed behaviour for people for whom dementia might be suspected but not yet diagnosed, or clients for whom dementia has been diagnosed and is progressing.
Early Changes
Memory: A person has difficulty recalling information or events, especially those that are more recent (short-term memories) rather than those from earlier in life (long-term memories).
Apathy: A person shows a persistent loss of motivation or interest in events or activities they have previously enjoyed
Delusion: False beliefs that something is true (different to a hallucination, which involves a sensory experience, in which a person can see, hear, smell, taste or feel something that is not there).
Triggers To Responsive Behaviours
If we can find out what the person living with dementia is reacting or responding to, we may be able to meet the need, thus reducing the distress and the behaviour.
How to reduce changed behaviours:
Work with the person, the family and the care team to build up a picture of why the person may be behaving differently and what helps to reduce that behaviour.
Care workers/the family/care teams:
Record your observations in the progress notes:
- What was happening right before the behaviour occurred?
- Who was involved?
- Who was affected by the behaviour?
- What was done about it and did it work?
Five Main Factors To Consider When Looking For Triggers
When we’re looking for triggers, there are five main factors to consider:
1) Health
People with dementia may change their behaviour if they feel unwell or uncomfortable because of their health conditions.
Nursing interventions assess:
- Are they in pain?
- Are they taking their medications correctly?
- Have they recently started/changed a new medication?
- Are they having trouble seeing or hearing?
- Are they tired? hot? or cold?
- Do they have a urinary tract infection (UTI) or any other type of infection?
- Do they drink enough water?
Care workers:
Report any signs/symptoms of illness or changes in behaviour to your supervisor and document them. They can organise a medical review and get the treatment that may be needed.
2) History
It is important to know the life history of the person living with dementia. In order to support them to live an enhanced quality of life, we need to know who they are as a person, the life they have led and prefer, and know what is meaningful to them.
The patient’s short-term memory is affected before their long-term memories. People with dementia often believe they live in a different time in their lives. If people confuse their present and their past, they may not recognise people in their lives. This can cause distress and changed behaviours.
Care workers:
If someone with dementia confuses you with a family member and starts to act inappropriately, report it to your supervisor. They may need to schedule another care worker.
In other situations, if the person thinks they know you, it might help to go along with it – it could be reassuring for them.
It’s important to know what works for each individual, so we have to get to know their histories.
Nursing interventions:
- Using prompts of past achievements and hobbies, such as pictures of those special events
- Label photos with people’s names
- Reporting to the supervisor if another care worker is needed
- Knowing what is individually meaningful for the person
3) Environment
In an attempt to reduce responsive behaviour, we can consider the environment of the person living with dementia.
There are many aspects of the physical environment that have the potential to impact a person living with dementia, causing distress and/or confusion.
Some environmental factors to consider include:
- Loud noise
- Clutter
- Poor lighting – shadows can be confusing
- Items that do not contrast in colour
- Mirrors can be confusing, should use a towel to cover them
- Bathrooms can be too white and reflect glare
- Nursing homes may not reorganise a familiar area to the person, speaking to family members
4) Tasks
In community care, engaging a person living with dementia in activities of daily living can have the potential to cause distress to the person.
The impact of dementia can cause the person to become overwhelmed by tasks they were once very capable of. Modifying tasks to match the person’s strengths and abilities can work toward reducing incidents of responsive behaviour.
Participating in a meaningful activity, like preparing dinner, can be beneficial for a person living with dementia. However, it can be overwhelming for a person living with dementia when they are asked questions that require decision-making.
To avoid overwhelming the person unnecessarily, review dementia nursing care plans and know what you need to do to support the person with dementia before you arrive at their home.
Care workers:
- Read the care plan or talk to your supervisor to understand what you need to do before attending the care service.
- Wear the uniform and your name tag at all times.
- Introduce yourself every time when you arrive at the person’s home.
- Give the person a choice such as asking if they would like a cup of coffee or tea.
- Encourage the person to participate in the daily activities together.
- Modifying tasks to match the person’s strengths and abilities.
- Do not correct them if they made a mistake doing a task you gave them.
5) Communication
A person’s ability to successfully communicate can be impaired by the impact of dementia. Impaired verbal communication results in frustration and confusion.
Here are some key points to consider for successful communication:
- Consider environmental noise
- Slow down your verbal communication
- Break tasks down into small steps
- Instructions should be delivered clearly and concisely
- Positive body language is important, gestures should match what is being said
- Maintain eye contact
- Visual cues may help a person with dementia to identify what they need or want
Nursing Interventions
Nursing interventions assess patient and family needs, develop a plan of care to meet those needs, and evaluate the patient’s response.
Nursing interventions should focus on the patient independence and the patient’s ability. To achieve functional ability by promoting safety, providing support and assistance with activities of daily living, and preserving as much cognitive function as possible.
Nursing interventions should be individualised to meet the needs of each person living with dementia. There is no one-size-fits-all approach to managing dementia.
Here are some common nursing interventions:
- Assess the person’s level of understanding
- Provide simple explanations
- Encourage patient to ask questions
- Use visual aids
- Television and radio programs
- Assist patient with making self-care activities
- Reality orientation techniques
- Utilize community resources
If the behaviour escalates – strategies for keeping yourself safe:
- Move away from the reach of the person
- Be calm and don’t overreact
- Try to distract and divert the person to something positive
- As a precaution, make sure you have an exit, do not box yourself into a corner
- Leave the person temporarily and come back later
- Call your supervisor
- Document the incident, the action you took and its outcome
If the person is hallucinating:
- Remember, for the person with dementia, what they see or hear is real to them
- Do not automatically assume they are hallucinating, investigate any suspicion the person with dementia may have which is causing them distress
- If they are happy in their reality, leave the situation alone.
- If they are distressed, acknowledge their feelings and let them know you are there to help
- Distract or divert to meaningful engagement
- Document and report to your supervisor
Disinhibited behaviour:
- Don’t overreact
- Remind them their behaviour is inappropriate
- Try to divert and distract them
- Give them something to fidget with
- If in public lead them to somewhere more private
Evening restlessness (Sundowning):
- Establish a routine for the person
- Increase the person’s exposure to natural daylight
- Encourage a short nap of up to 40 mins during the day
- As evening draws, darken and reduce noise
- Encourage the person to help with general tasks
- Music may be soothing
- For some, a warm bath or shower may help
Depression – can look a lot like symptoms of dementia, yet is treatable. Signs and symptoms to look out for:
- Unusually withdrawn and emotional
- No appetite or energy
- Losing interest in things they usually enjoy
- Talking about self-harm or suicide
Conclusion
If you are caring for someone with dementia, it is important to be patient, understand their limitations, and provide them with the support they need to maintain as much independence as possible.
Nursing diagnosis for dementia can be difficult. However, by understanding the basics of the disease and the available interventions, you can provide better care for your patients. Thanks for reading!
Please feel free to contact me if you have any questions.